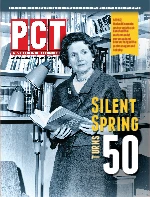
 Rachel Carson’s “Silent Spring” was indeed a landmark book that changed the course of history, contributing to the formation of the U.S. Environmental Protection Agency, and ultimately, for better or worse, a flood of federal and state regulations on pesticide use. Her call for restraint in pesticide use was written in a very persuasive and humble way which elicited broad appeal among the public (and still does).
Rachel Carson’s “Silent Spring” was indeed a landmark book that changed the course of history, contributing to the formation of the U.S. Environmental Protection Agency, and ultimately, for better or worse, a flood of federal and state regulations on pesticide use. Her call for restraint in pesticide use was written in a very persuasive and humble way which elicited broad appeal among the public (and still does).
“Silent Spring” was actually the culmination of a movement that started a long time ago. From the turn of the 20th Century through late 1950s, the idea of a “web of life” began to take hold in America, in which all creatures depended upon one another for their mutual survival. The underlying foundation of this awareness was that humans weren’t really “above” nature, but a part of it. Therefore, when Rachel Carson’s 1962 classic came out, which was a quietly shocking tale about the widespread pesticide poisoning of humans and nature, there was a powerful and visceral reaction to it. Her book sparked a public outcry for governmental regulation to protect the environment, not just from future exploitation, but for its own innate value. Carson had unwittingly launched the modern idea of environmentalism: a political movement that demanded government not only preserve the Earth and its inhabitants, but also take action to regulate and punish those who mistreat it.
Perception vs. Reality. To me, the worst thing about “Silent Spring” is not what it actually says, but what people perceive it says. Some have concluded that Rachel Carson’s message was that pesticides are evil in themselves — some sort of social ill that needs to be removed. That is, some have concluded that she meant pesticides are inherently bad, or flawed, or unnatural, and should not be allowed in society (like atomic bombs). That point of view, I think, is misguided at best, and dangerous at worst.
We need to keep in mind that pesticides are public health tools. As a public health entomologist, I have seen first-hand the devastating effects of arthropods and the diseases they cause. Through the years when I was at the Mississippi Department of Health, we investigated and tried to manage disease clusters and outbreaks due to Rocky Mountain spotted fever, St. Louis encephalitis, eastern equine encephalitis and West Nile virus. I have personally visited with grieving family members of those who died from these diseases, as well patients who are now permanently disabled from them, so no one is going to tell me that pesticides are not important in public health and effective disease prevention.
 Some of the earliest public health efforts to better human health and well-being were geared toward filth fly and mosquito control, and often included basic sanitation measures such as installation of screen-wire windows and doors, clean water supply, sewage disposal and insect breeding site elimination. After World War II, these efforts also included (and maybe too much so) copious spraying with pesticides such as DDT. Modern public health still employs these tools and methods, as well as the addition of immunizations; better, more effective and targeted use of pesticides; and high-tech disease surveillance and control techniques.
Some of the earliest public health efforts to better human health and well-being were geared toward filth fly and mosquito control, and often included basic sanitation measures such as installation of screen-wire windows and doors, clean water supply, sewage disposal and insect breeding site elimination. After World War II, these efforts also included (and maybe too much so) copious spraying with pesticides such as DDT. Modern public health still employs these tools and methods, as well as the addition of immunizations; better, more effective and targeted use of pesticides; and high-tech disease surveillance and control techniques.
In the last two decades, there has been a drift toward increased scrutiny of pesticide use, with some segments of the population demanding elimination of most (if not all) uses of the substances. However, it is important to realize that — from the public health perspective — pesticides are critical tools to manage vector-borne infectious diseases.
Why we need insecticides. Infectious diseases are making a strong comeback after a lull in the years following World War II. The ability of disease germs to adapt to the human defense system and intense pressure from antibiotic use, combined with changes in society, have contributed to this comeback. Also, there are now several “new” or emerging diseases, including SARS, Legionnaires’ disease, Lyme disease, ehrlichiosis, toxic shock syndrome and Ebola hemorrhagic fever. In just the last three decades we have seen the appearance of a new strain of bird influenza that attacks humans, a human form of “mad cow” disease and new drug-resistant forms of Staphylococcus aureus. These new or emerging infectious diseases have raised considerable concern in the medical community about the possibility of widespread and possibly devastating disease epidemics.
Humans are now in a precarious situation. The entire ecosystem — including plant and animal life on earth — is being negatively affected by human civilization. People once lived in far-removed, relatively isolated groups. Now we are all essentially one large community. Further, things such as population increases, building cities in/near jungles, and widespread and frequent international air travel are providing the opportunity for an outbreak of a great plague.
For example, the number of international departures from U.S. airports doubled from 20 million to nearly 40 million between 1983 and 1995. A person hiking in the Amazon jungles today might be in New York City (or your town) tomorrow. Should one or more new emerging vector-borne diseases begin to spread, control of the epidemic would be difficult.
As an example of quick spread of disease agents, consider swine flu, which was first discovered in Mexico in late March 2009, and by the first week of May (six weeks later), had spread to many places worldwide, from New York to New Zealand. If an emerging disease agent is a virus, specific treatments are unavailable (or, at least, untested against most arboviruses). The only way to stop a viral vector-borne illness is to kill the vectors to a low enough level to interrupt virus transmission. If the vector is a flying insect, control of an epidemic is even harder. Compounding all of this, many insect species are resistant to many of the traditional insecticides used to control them.
 Mosquito control through the years: This 1965 photograph from the Centers of Disease Control and Prevention depicts an entomologic field technician using an aspiration suction tube in order to trap adult mosquitoes from the interior of a drainage pipe. “Keeping close tabs on potential mosquito vector populations is essential in maintaining control over a possible epidemiologic outbreak of vector-borne diseases such as Dengue fever, malaria or West Nile virus,” CDC writes. Mosquito control through the years: This 1965 photograph from the Centers of Disease Control and Prevention depicts an entomologic field technician using an aspiration suction tube in order to trap adult mosquitoes from the interior of a drainage pipe. “Keeping close tabs on potential mosquito vector populations is essential in maintaining control over a possible epidemiologic outbreak of vector-borne diseases such as Dengue fever, malaria or West Nile virus,” CDC writes. |
Pesticides are designed to kill things and therefore should (rightly) be considered as poisons. But the EPA registration process, requiring many years of product testing and review, helps ensure that EPA-registered products are safe when used according to their label directions. Millions of dollars are invested in testing pesticide products — before they ever reach the consumer — for their relative safety to humans and the environment. Prospective pesticides are tested for harmful effects to adults, children, the unborn, as well as the environment. Some people still claim that pesticides are ruining the environment and causing widespread disease such as cancer in the human population, but evidence for these claims is lacking. Wildlife is abundant. There are more deer and wild turkeys in the U.S. now than at the beginning of the 20th century. People are healthier and living longer. Both incidence and death rates from all cancers combined declined significantly in the most recent time period for men and women overall and for most racial and ethnic populations.
The Future. Pesticides are important for human survival. They are essentially environmental medicines needed to correct insect imbalances. Not only are they needed for crop protection, but as public health tools. Pesticides are needed to combat vector-borne diseases that may arise, or any re-emergence of existing diseases (such as malaria, dengue, etc.). Certainly, Integrated Pest Management and other strategies to reduce pesticide use are in order, but in many cases insect populations explode and are unmanageable by non-chemical methods. We must have pesticides readily available for use. Not only do we need pesticides, we need a wide variety of them with various labeled uses.
 Furthermore, registrations for many pesticide uses are considered “minor uses” by EPA and chemical companies, and thus, not much attention is paid to them. In fact, many of these minor-use registrations are being dropped totally. Even though a “public health” use may be allowed by the EPA for a particular pesticide, the pesticide may not be available if the company decides (due to EPA review or anti-pesticide group harassment) to quit making it. This is a worrisome trend. We need all legitimate pesticide registrations to remain in effect as part of public health’s repertoire of weapons against insect pests. “Silent Spring” was indeed an important turning point in the history of pesticides and public attitudes toward them, but let’s not take that sentiment too far.
Furthermore, registrations for many pesticide uses are considered “minor uses” by EPA and chemical companies, and thus, not much attention is paid to them. In fact, many of these minor-use registrations are being dropped totally. Even though a “public health” use may be allowed by the EPA for a particular pesticide, the pesticide may not be available if the company decides (due to EPA review or anti-pesticide group harassment) to quit making it. This is a worrisome trend. We need all legitimate pesticide registrations to remain in effect as part of public health’s repertoire of weapons against insect pests. “Silent Spring” was indeed an important turning point in the history of pesticides and public attitudes toward them, but let’s not take that sentiment too far.
The author is a public health entomologist and author of The Physician’s Guide to Arthropods of Medical Importance. E-mail him at jgoddard@giemedia.com.
Explore the September 2012 Issue
Check out more from this issue and find your next story to read.
Latest from Pest Control Technology
- Rentokil Terminix Expanded in Key Markets with 2024 Acquisitions
- In Memoriam: Joe Cavender
- Certus Acquires Green Wave Pest Solutions
- Liphatech Adds Alex Blahnik to Technical Team
- Do the Right Sting: Stinging Insect Identification, Management, and Safety
- VAGA's 8th Annual Veterans Thanksgiving Appreciation Dinner
- Clark's Blair Smith on the Response to Increased Dengue Fever Cases in Southern California
- WSDA, USDA Announce Eradication of Northern Giant Hornet from U.S.





